The Inheritance Patterns of Some Rarer Forms of SMA
The Inheritance Patterns of Some Rarer Forms of SMA
You can:
- Download a printed pdf version of this information here >
- Ask us to send you a printed version: publications order form >
Who this is for
This guide is for anyone who wants to understand more about why there are different inheritance patterns for different genetic conditions. It explains what this pattern is for these rarer forms of SMA:
- Distal Spinal Muscular Atrophy type V (DSMA-V)
- Spinal and Bulbar Muscular Atrophy (SBMA) – also known as Kennedy’s Disease
- Spinal Muscular Atrophy with Lower Extremity Predominance (SMA-LED)
- Spinal Muscular Atrophy with Progressive Myoclonic Epilepsy (SMA-PME)
- Spinal Muscular Atrophy with Respiratory Distress 1 (SMARD1)
- X-linked Infantile Spinal Muscular Atrophy
Genetic conditions are caused by alterations in our genes which prevent the gene from working properly.
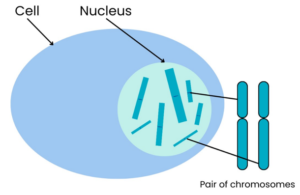
Our bodies are made up of many millions of cells. Nearly all cells have a structure called the nucleus, which contains chromosomes that contain genes.
Chromosomes are compact bundles of DNA. (See Box 1 for an explanation of DNA.)
A gene is a specific section of DNA.
Body cells have two copies of each chromosome, as we inherit one copy from each parent.
We all have 46 chromosomes in each cell in our body, arranged in 23 pairs. There are two exceptions to this: our red blood cells do not have any chromosomes, and our egg and sperm cells only have one of each pair of 23 chromosomes.
This means we have two copies of every gene (except in the egg and sperm cells where there is only one copy).
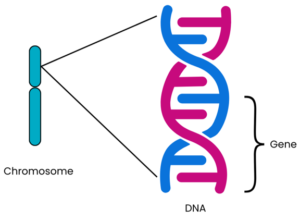
Genes are a sequence of code (called base pairs) that are read by the body to make proteins (see Box 1 for more information). Our cells need proteins for their structure, survival and to work correctly. We each have approximately 20,000 different genes making different proteins in our bodies¹‾². Each protein made by a different gene has its own unique function. The structure of the protein, and therefore its function, is determined by the order in which the base pairs are arranged in that particular gene. Usually, there are two copies of each gene on each chromosome pair: one inherited from each parent.
Sometimes a gene can contain an alteration known as a mutation. Genetic conditions occur when a mutation within a gene affects how the protein in our bodies is produced and how it works.
DNA is often described as a recipe book, or a set of instructions, because it contains the information needed for a person to grow and develop.
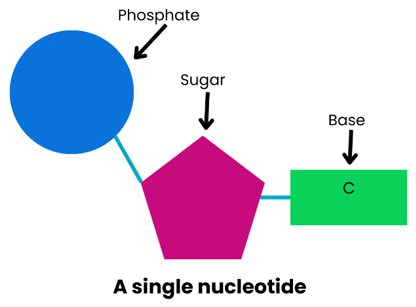
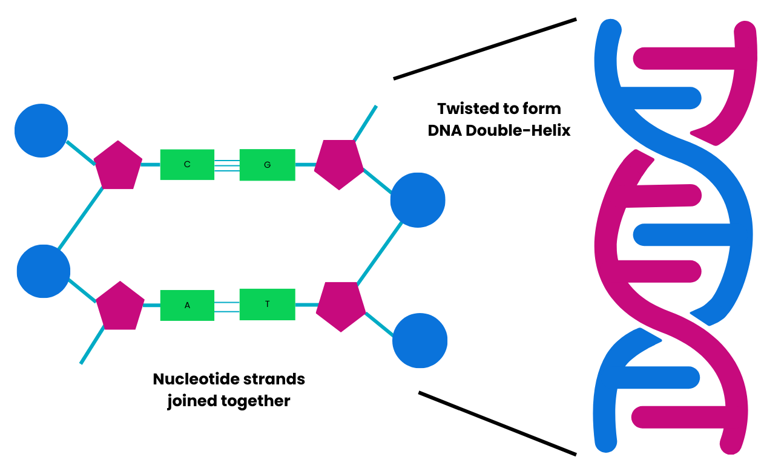
DNA is made up of lots of nucleotides joined together. Each nucleotide contains a phosphate, a sugar and a base. The phosphate and sugar are always the same but the base varies in each nucleotide. The base can be one of four: adenine (A), guanine (G), cytosine (C), or thymine (T).
These bases pair up: A with T and C with G. The order in which these pairs of bases are arranged affects how the ‘recipe book’ information is read. The joined base pairs hold the nucleotides together in strands that twist together to form the DNA double-helix shape.
We all have 46 chromosomes in each cell in our body, except for egg and sperm cells. These are arranged in 23 pairs:
- 22 of the pairs are non-sex chromosomes, known as autosomes. These are found in both males and females.
- The 23rd pair consists of two sex chromosomes, which determine your sex. Females usually have two X chromosomes (XX), and males an X and a Y chromosome (XY).
An autosomal condition means that the gene alteration causing the condition is located on one of the autosomal chromosomes. It is not on one of the two sex chromosomes.
When a condition is autosomal dominant, only one copy of the altered gene is needed to pass on the condition.
Autosomal dominance is the inheritance pattern most often seen in:
- Distal Spinal Muscular Atrophy Type V (DSMA-V) >
- Spinal Muscular Atrophy with Lower Extremity Predominance (SMA-LED)>
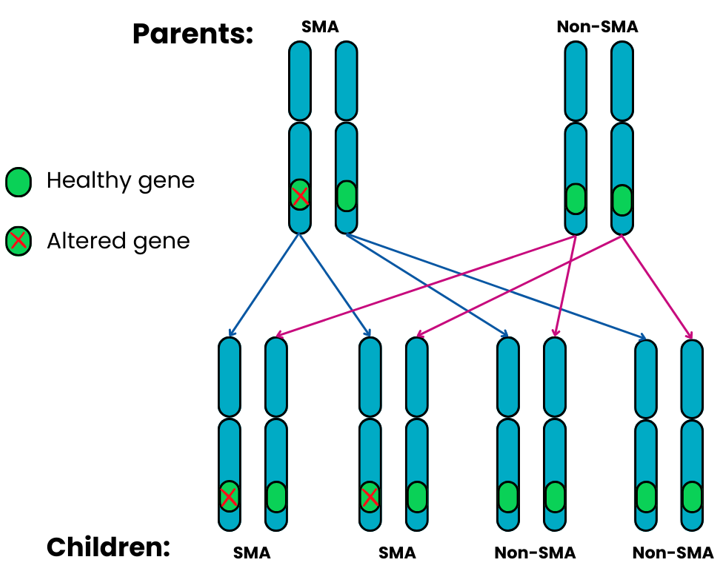
The two diagrams below show what the chances are of parents passing on their rare form of SMA to their children if the inheritance pattern is autosomal dominant. For each pregnancy, these chances are the same.
Autosomal dominant Family 1: one parent has SMA and the other does not.
For each pregnancy, the chances are:
- Child will have SMA: 2 in 4 chance (50%)
- Child will not have SMA: 2 in 4 chance (50%)
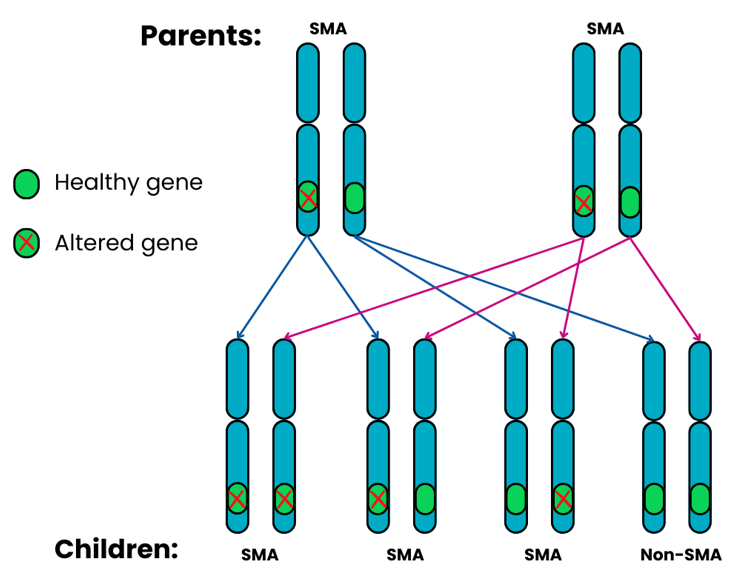
Autosomal dominant Family 2: both parents have SMA.
If both parents have SMA and their child inherits two dominant genes, one from each parent, this can cause a much more severe form of SMA and possibly other difficulties for the child as well.
For each pregnancy, the chances are:
- Child will have SMA: 3 in 4 chance (75%)
- Child will not have SMA: 1 in 4 chance (25%)
We all have 46 chromosomes in each cell in our body, except for egg and sperm cells. These are arranged in 23 pairs:
- 22 of the pairs are non-sex chromosomes, known as autosomes. These are found in both males and females.The 23rd pair consists of two sex chromosomes, which determine your sex. Females usually have two X chromosomes (XX), and males an X and a Y chromosome (XY).
An autosomal condition means that the gene alteration causing the condition is located on one of the autosomal chromosomes. It is not on one of the two sex chromosomes.
A recessive condition means that both of the pair of genes are altered.
This is the inheritance pattern most often seen in:
With an autosomal recessive condition:
- a person will only have the condition if they inherit two altered copies of the altered gene – one from each parent
- a person who carries one altered copy of the gene and one healthy copy will not have the condition but is a carrier. They do not have any symptoms, but the altered gene can be passed on to their children.
The chances of children being carriers or having a rare form of SMA will depend on whether their parents have the condition or are carriers.
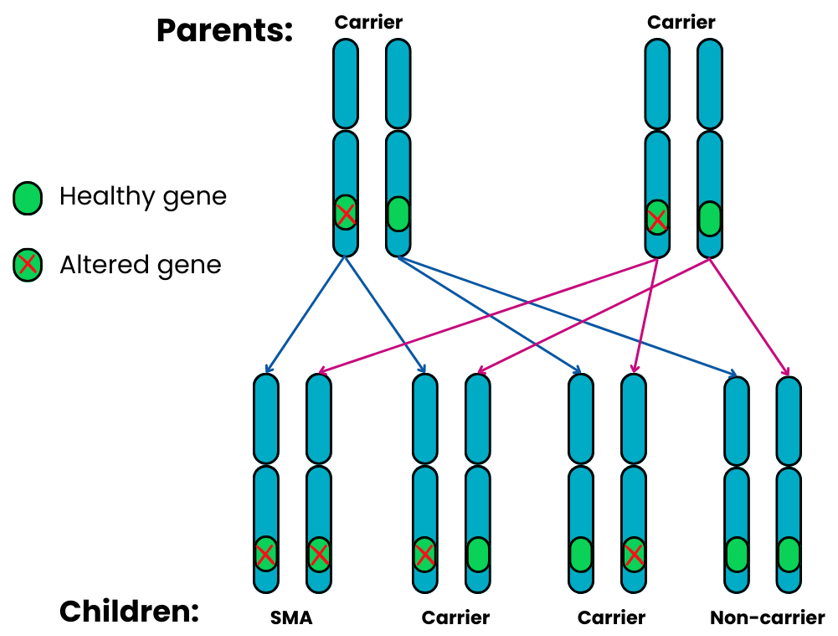
Autosomal recessive Family 1: both parents are carriers.
For each pregnancy, the chances are:
- Child will have SMA: 1 in 4 chance (25%)
- Child will not have SMA but will be a carrier: 2 in 4 chance (50%)
- Child will not have SMA and is not a carrier: 1 in 4 chance (25%)
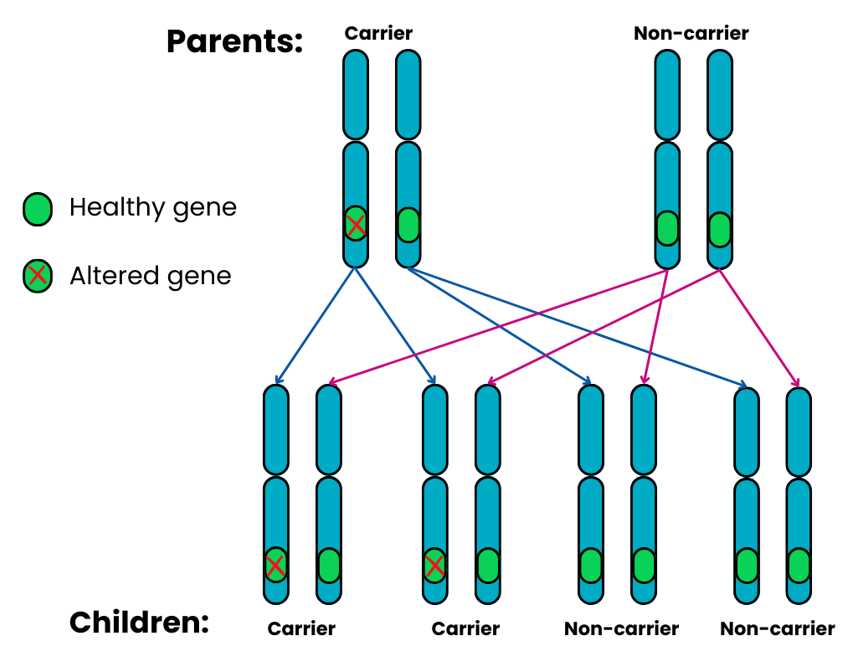
Autosomal recessive Family 2: one parent is a carrier, the other does not have SMA & is a non-carrier.
For each pregnancy, the chances are:
- Child will have SMA: not possible (0%)
- Child will not have SMA but will be a carrier: 2 in 4 chance (50%)
- Child will not have SMA and will not be a carrier: 2 in 4 chance (50%)
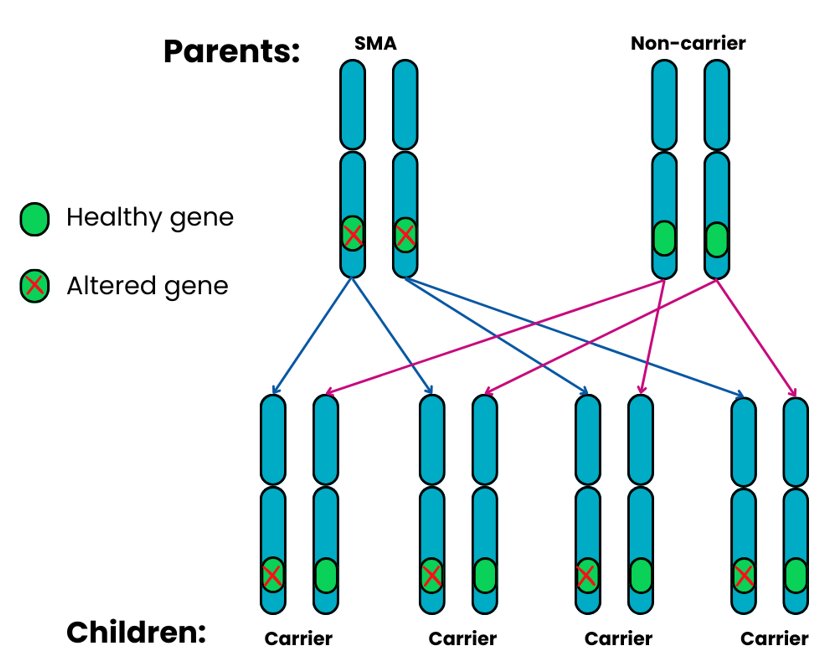
Autosomal recessive Family 3: one parent has SMA, the other does not have SMA and is a non-carrier.
For each pregnancy, the chances are:
- Child will have SMA: not possible (0%)
- Child will not have SMA and will not be a carrier: not possible (0%)
- Child will not have SMA but will be a carrier: 4 in 4 chance (100%)
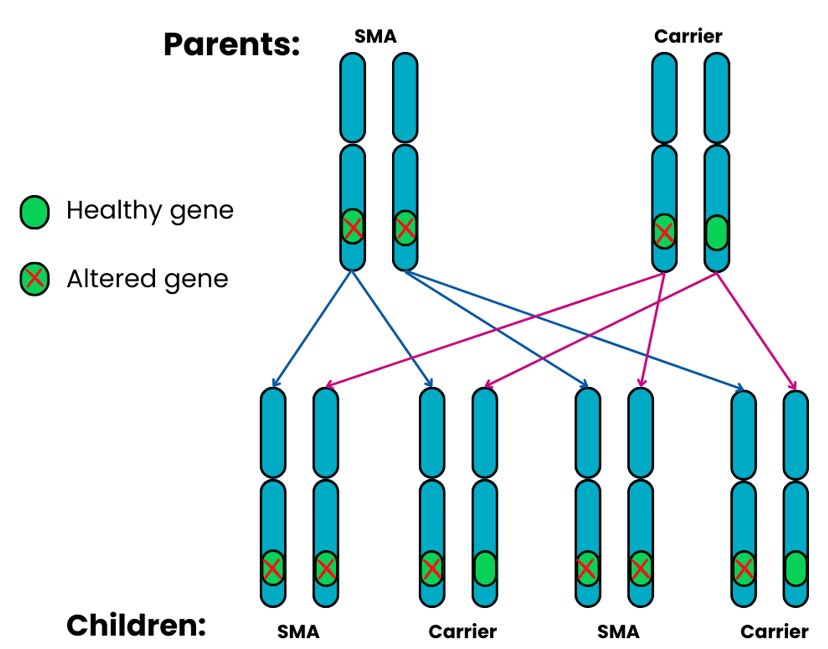
Autosomal recessive Family 4: one parent has SMA, the other is a carrier.
For each pregnancy, the chances are:
- Child will not have SMA and will not be a carrier: not possible (0%)
- Child will have SMA: 2 in 4 chance (50%)
- Child will not have SMA but is a carrier: 2 in 4 chance (50%)
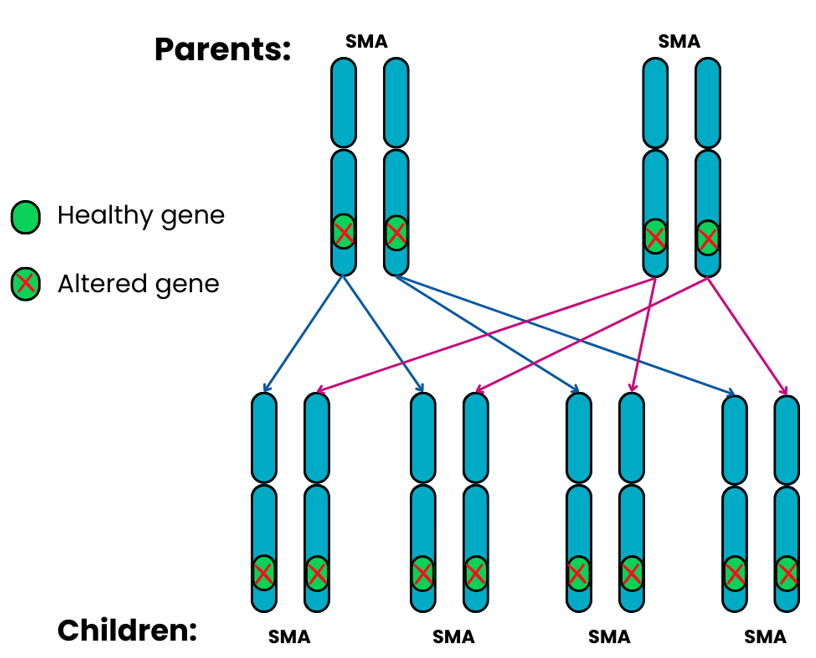
Autosomal recessive Family 5: both parents have SMA.
For each pregnancy, the chances are:
- All the children will have SMA: 4 in 4 chance (100%)
We all have 46 chromosomes in each cell in our body, except for egg and sperm cells. These are arranged in 23 pairs:
- 22 of the pairs are non-sex chromosomes, known as autosomes. These are found in both males and females.
- The 23rd pair consists of two sex chromosomes, which determine your sex. Females usually have two X chromosomes (XX), and males an X and a Y chromosome (XY).
In an X-linked recessive pattern of inheritance, the altered gene is on the X chromosome. It is not found on the shorter, male-specific Y chromosome. Males only have one X chromosome and therefore only one copy of the gene. This means that if they have one altered copy then they have no other healthy copy. Males are therefore much more frequently affected by X-linked disorders than females.
Females with one healthy copy and one altered copy of the gene do not usually have any symptoms. Some do though have a very mild form of the condition. However, the altered gene can be passed on to their children. As a result of this they are called carriers.
This is the inheritance pattern most often seen in:
- Spinal and Bulbar Muscular Atrophy (SBMA) – also known as Kennedy’s Disease >
- X-linked Infantile Spinal Muscular Atrophy >
The chances of children being carriers or having a rare form of SMA will depend on whether their parents have the condition or are carriers.
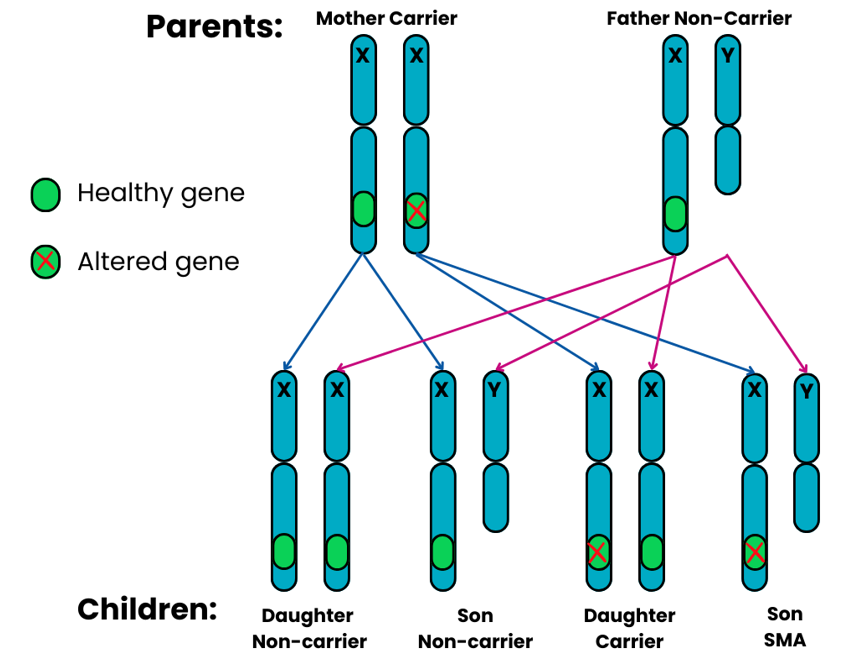
X-linked recessive Family 1: the mother is a carrier, the father is not a carrier and doesn’t have SMA.
For each pregnancy, the chances are:
- Daughters will have a 1 in 2 chance (50%) of not having SMA and not being a carrier
- Sons will have a 1 in 2 chance (50%) of not having SMA and not being a carrier
- Daughters will have a 1 in 2 chance (50%) of being a carrier
- Sons will have a 1 in 2 chance (50%) of having SMA
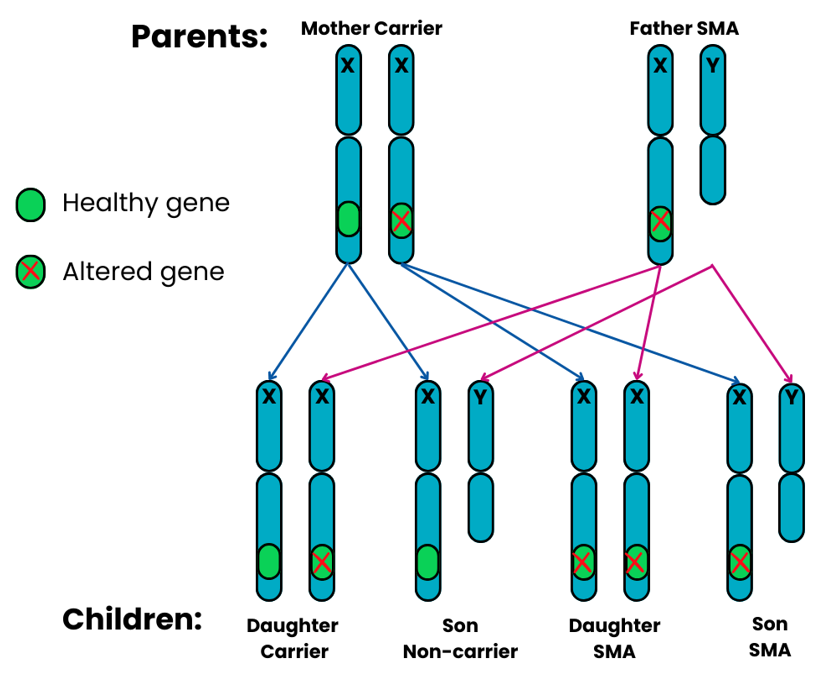
X-linked recessive Family 2: the mother is a carrier, the father has SMA.
For each pregnancy, the chances are:
- Daughters will have a 1 in 2 chance (50%) of being a carrier
- Sons will have a 1 in 2 chance of not having SMA and not being a carrier
- Daughters will have a 1 in 2 chance (50%) of having SMA
- Sons will have a 1 in 2 chance (50%) of having SMA
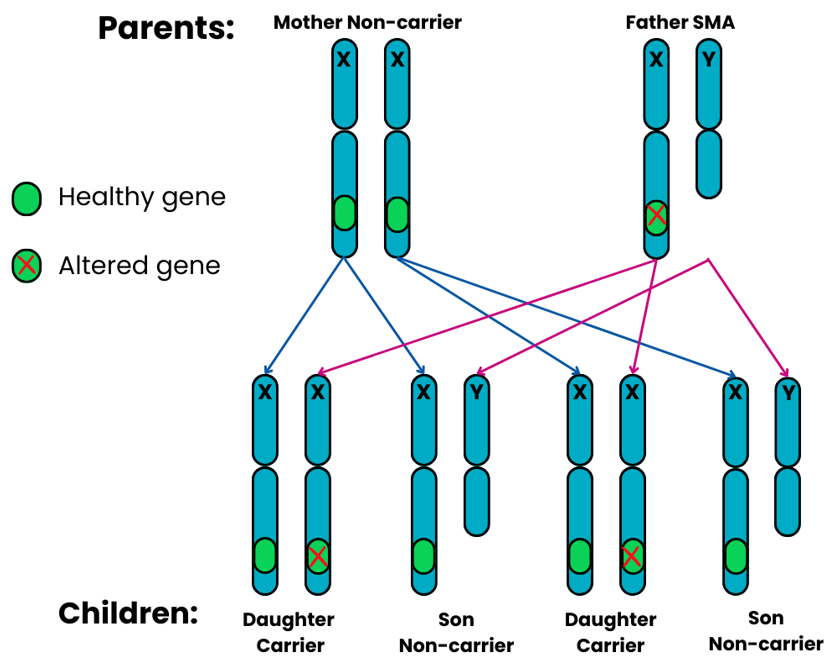
X-linked recessive Family 3: the mother does not have SMA and is not a carrier, the father has SMA.
For each pregnancy, the chances are:
- Daughters will have a 2 in 2 chance (100%) of being a carrier
- Sons will have a 2 in 2 chance (100%) of not having SMA and not being a carrier
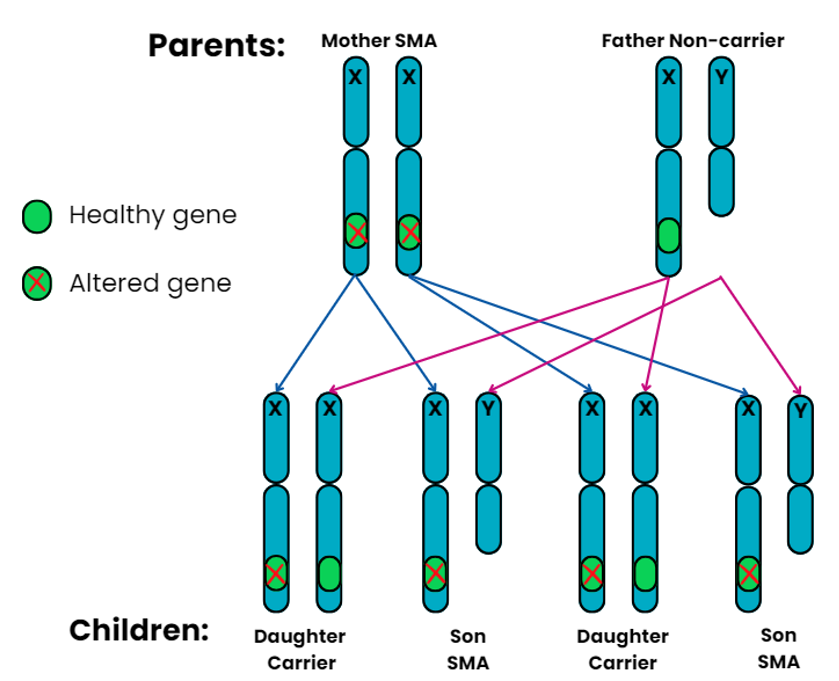
X-linked recessive Family 4: the mother has SMA, the father does not have SMA and is not a carrier.
For each pregnancy, the chances are:
- Daughters will have a 2 in 2 chance (100%) of being a carrier
- Sons will have a 2 in 2 chance (100%) of having SMA
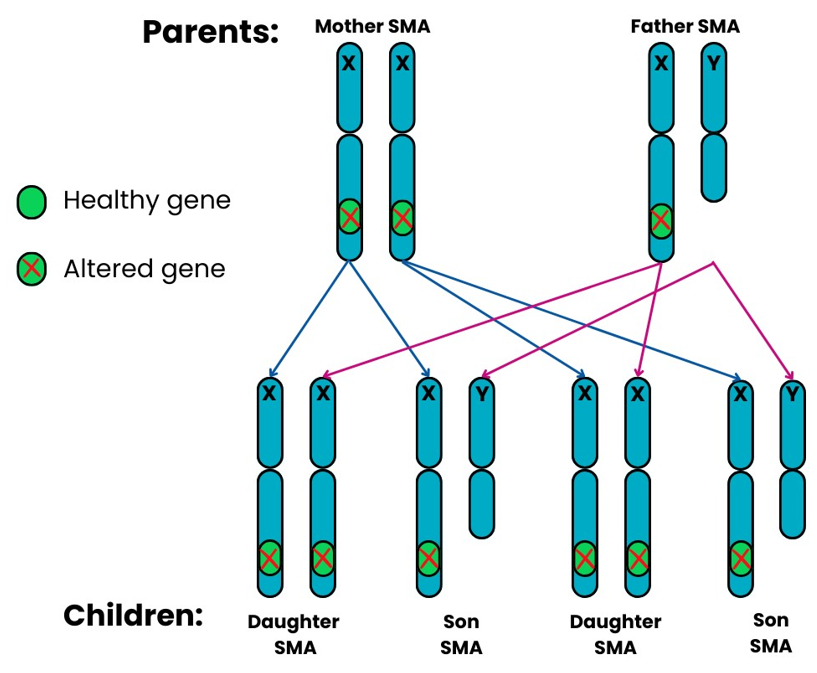
X-linked recessive Family 5: both parents have SMA.
For each pregnancy, the chances are:
- All the children will have SMA
In most cases of SMA, the gene change or changes are clearly inherited from one or both parents. They may themselves have no symptoms of SMA. This is particularly the case in autosomal recessive or X-linked recessive forms. In rarer cases, however, the genetic cause for SMA may not be present in either parent or is not clearly present in the cells analysed in the carrier test. In other words, it may be a new gene change in the affected individual. This situation can be caused by a “de novo” mutation or something known as “germline mosaicism” in a parent.
-
De Novo
De novo means “from the beginning”. It is a type of alteration that occurs either
- when an individual sperm or egg is made, or
- when a sperm fertilises an egg, or
- when cells are dividing after fertilisation.
The most likely reason is an error in the making of the sperm or egg cell. As it occurs at this stage, the alteration will not be detected in either of the parents.
-
Germline Mosaicism
This is when an individual produces sperm or egg cells that differ in their genetics from all the other cell types in the body of that person. If the SMN1 gene is affected in this way, the sperm or eggs of that individual can have an altered SMN1 gene. This would go undetected by the carrier test.
These rare scenarios can have implications for the chance of SMA affecting a future pregnancy. They show that carrier testing for genetic conditions will never be 100% accurate. They highlight the importance of having genetic counselling specific to your own circumstances.
The laboratory and your clinical and genetics team can discuss any limitations of the testing with you. They will also try to ensure the testing for your family is as accurate as possible.
The genetics of SMA are complex. Also, for a small number of people, their genetic circumstances are not clear. For example, for some people, a diagnosis of ‘adult onset SMA’ is made even though the genetic cause of their SMA has not been identified.
Genetic counselling is with a healthcare professional who has expert training in genetics. They will aim to explain results from your genetic testing in an easily understandable way. They will answer any questions you might have about the genetic aspects of the diagnosis.
People often discuss:
- implications or options for a future pregnancy
- if the diagnosis should be discussed with other family members who might wish to seek genetic counselling.
More Information about Genetics and Genetic Testing:
Phone: 0207 704 3141.
Support:
Phone 01789 267520.
- International Human Genome Sequencing Consortium (2004) ‘Finishing the euchromatic sequence of the human genome’, Nature, 431, pp. 931-945.
- Pennisi, E. (2012) ‘ENCODE project writes eulogy for junk DNA’, Science, 337(6099), pp. 1159-1161.
Was this page useful?
 Version 6
Version 6
Author: SMA UK Information Production Team
Last Reviewed: September 2025
Next Review: July 2028
Links last checked: September 2025
This page, and its links, provide information. This is meant to support, not replace, clinical and professional care.
Find out more about how we produce our information.
